Diabetes for Dummies, aka Diabetes Dirge
The Red Queen contracts out Diabetic Dirge
This started out as an in-depth review of current diabetes mellitus (aka type 2 diabetes, T2D) models and how they view metabolic health. Several authors, (DeFronzo 2009)(1)((1. Defronzo, R. A. (2009). Banting lecture. From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes, 58(4), 773-95. http://doi.org/fd98q8)) and (Schwartz 2019)(2)((2. Schwartz 2019. Bonadonna, R. C., Groop, L. C., Zych, K., Shank, M., & DeFronzo, R. A. (1990). Dose-dependent effect of insulin on plasma free fatty acid turnover and oxidation in humans. American Journal of Physiology-Endocrinology and Metabolism, 259(5), E736-E50. http://doi.org/dsk2)), used musical names to describe T2D players, e.g. Triumvirate Trio, Dysharmonious Quintet, Setaceous Sextet, and so on. Since their analogy emphasized interconnectedness, it seemed natural to continue in that fashion. What do you think of “Diabetes Dirge – Sugar Blues, Metabolic Quintet & Chronic Symphony” for a title?
Another T2D model pops-up
As my research progressed, I ran into another current T2D model from the American Association of Clinical Endocrinologists (AACE) aimed at pharmacological interventions with some thoughts about prevention, but no mention of metabolic health or flexibility.1
The more I read, the more I realized that T2D studies were not focused on creating metabolic health, but instead on targeting specific areas to interact with medications. The emphasis was on band aids for metabolic syndrome. And, each study came with a caveat: the perplexing conclusion that more studies were required. (Kostoff 2019)2
The list of references is growing
How is an ever-expanding medical literature using more technical language going to help me live a healthy life? Is this vast opus of data applicable to my lifestyle and daily habits? Could it be that the progression of diabetes plays a role in many chronic diseases that destroy metabolic health?
How can I use all this information to improve my health?
Diabetes is like the manipulative Red Queen that created so many of Alice’s woes as she wandered through Wonderland. Does T2D create a funeral song, a dirge, for our metabolic health? Where is the formula for me to create useful knowledge for metabolic flexibility? If there is a progression of disease to chronic conditions is there a way to reverse the illness? (Johnson 2018)3
Is there a simple question that if answered might help understand T2D?
As I wade through the literature and competing theories I ask myself this basic question. I think it will help me understand what’s going on with T2D:
“Why does resting homeostasis finely tune and tightly control blood glucose, quickly raises it to exercise, but fights to lower it after eating?”
A lot of questions. Some with easier answers than others. So, let’s start by defining terms.
Diabetes Mellitus (DM) – dynamic illness
In recent decades advances in technologies and methodologies have broadened and deepened our understanding of DM (aka, type 2 diabetes, T2D). We know that diabetes impacts many organs, destroys metabolic heath and develops over decades before it is diagnosed. Precision in measuring genetic and biochemical interactions has increased, the theory has expanded, and scientists have created a unifying theory of symptoms.
T2D, one disease or many illnesses?
T2D progresses over decades. As different organs are compromised their symptoms are used to characterize its etiology. For example, how over time the pancreas becomes unable to properly secrete insulin. This approach leads to various treatment regimens because the lungs fail, the eyes fail, etc. (van Ommen 2018)4 Thus it becomes necessary for current symptomatic models of T2D to incorporate the hypothalamus, pancreatic α & β-cells, hepatic processes, muscle & adipose tissues, the immune system, and the intestinal tract.
Is T2D a disease or a set of symptoms?
Disease in these major systems is the visible effect of a perturbed, integrated and complex metabolic-feedback system. (Bonadonna 1990)5 What disturbs the body’s finely regulated insulin secretion? Sugar and Fat: Glucotoxicity and lipotoxicity. …
Wait a minute, I think we’re going down the wrong rabbit hole here. We’re complicating the explanation. If T2D symptoms are understandable, then can it be based on how you feel, instead of abstruse words? How can we make sense, make useful choices about metabolic health from all this technical jargon?
After that mouthful did you need a bathroom break or a drink?
I’ll admit to looking up each of the words marked in red in the above paragraphs to find similar words, synonyms, for writing. I still don’t fully understand them or what they’re doing. However, after sketching out some thinking on insulin and glucose, I found something unexpected with diabetes synonyms: polyuria (frequent urination) and polydipsia (frequent thirst). You might not have been surprised that these are T2D names. However, you might not know they are hallmarks of kidney disease and its associated hypertension.
In our madness for staying hydrated are we covering up an important symptom of T2D? Is our ever-present thirst driving consumption of sugary drinks? Are we caught up in a vicious cycle?
But isn’t the vicious cycle also one of more and more complicated words convoluting upon themselves? Of more and more data and information and less useful knowledge? Isn’t much of what’s being published confounded and confused? Doesn’t the confusion start with not clearly stating what a normal body should be like? Is that even possible?
What is a normal human?
In my dim memory I recall going to the high school chemistry lab and setting up the weekly experiment. There were specific instructions to establish initial conditions. You ignited the Bunsen burner or mixed the reagents and voilà—the expected results. But is it so easy to set up controlled situations for humans? What are the initial conditions?
Empty stomach or bellyful?
An otherwise well-conducted study starts off with a motivational statement that is pertinent to how we model normal physiology. In this research paper the authors explained that understanding how humans react to fatty acids (plasma lipoproteins) in the blood after eating fats is their goal. They explain that “human beings, by eating regular meals, spend most of the time in the postprandial phase (after eating). Consequently, this state is presumably more representative of the physiological status than the fasting situation.” (Bysted 2005, added emphasis)6
When did snacking start?
This might be the current situation due to modern snacking, but ancestral living probably resulted in the exact opposite condition. Didn’t humans evolve with hunger in their bellies? Assuming the body has just eaten radically alters blood glucose levels. This is especially so if you’ve eaten carbohydrates and if there’s frequent snacking. Should we adopt the model of an empty stomach or bellyful?
Fasting or snacking?
In a fasted human, insulin is low and glucose is tightly regulated. In contrast, in the absorptive phase after ingesting carbohydrates both insulin and glucose spike upwards. This is a dynamic response to a challenge and whether homeostasis7 is restored or not is a measure of illness or health. They are two different worlds. Is the snacking human our grounded condition to model?
Glucose (monosaccharide) or Sugar (disaccharide)?
The human body only has 5 grams of glucose circulating in the bloodstream—that’s a teaspoon! (Unwin 2017)8 In humans glucose, all that is needed by the body, is created by the liver and kidneys. There is no need to consume sugar. Sugar is not ‘natural’ to humans. Sugar is glucose and fructose—it comes from sugar cane.
Why glucose?
Why do our bodies use glucose (dextrose)? Because glucose does not bind as much as fructose and galactose to proteins.9 Blood proteins, like hemoglobin, when bound to monosaccharides (simple sugars) form advanced glycation end (AGE) products that are not healthy. (DiNicolantonio 2018)10 Glycated hemoglobin protein A (hbA1c) is used as a measure of diabetic sugar intolerance (impaired glucose tolerance, IGT).
Sugar by any other name would be as sweet
There are over 100 names for sugar11 and similarly for maltodextrin (a polysaccharide).12 So, which type of sugar is being studied? Have you heard the term glucotoxicity13 being bandied about?
Metabolic flexibility or metabolic syndrome (MetS)
Metabolic syndrome (MetS) is a cluster of five body measurements. Three out of the five symptoms, “elevated waist circumference, elevated triglycerides, reduced high-density lipoprotein cholesterol, elevated blood pressure and elevated fasting plasma glucose” qualifies as MetS. (Nilsson 2019)14
Are the studies answering the questions we need to ask?
So, in studies why are we using individuals that are metabolically inflexible? How are we guiding ourselves to health by using subjects that have insulin resistance (IR)? Insulin resistance makes these subjects unable “to adapt metabolism15 to the fasted-to-fed state transition.” (Hue 2009)16(Kelly 2000)17
Instead of the absence of markers, why can’t we have a positive definition of metabolic health?
This goes to the core issue of creating a positive definition of health, instead of our current focus on the absence-of-disease symptoms. It’s time for a shift. Let’s integrate mind, body and soul. (Huber 2016)18 “Embracing health as a system (i.e., including systems biology concepts and technologies), the development of disease from health as a continuum.” Perhaps by doing so we can shift from sick-care to health-care, to P4-medicine (Predictive, Personalized, Preventive, and Participatory).” (Wendimagegn 2019)19
Sitting or walking?
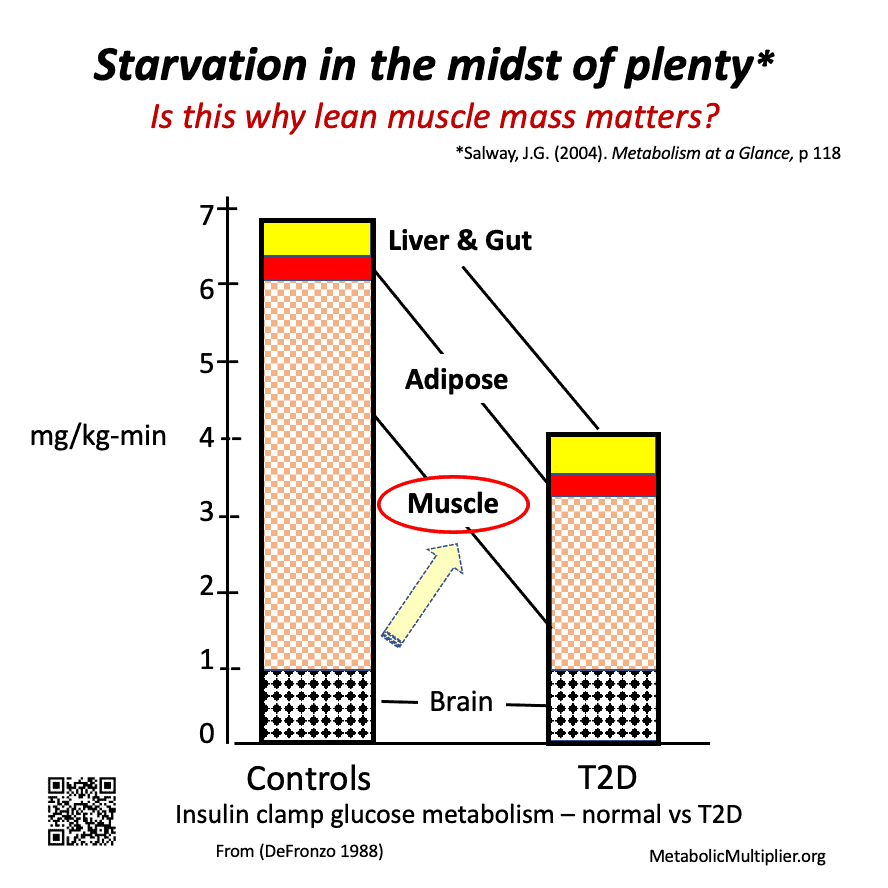
Defronzo in 198821 Their metabolic health is impaired.
“It would appear that owing to this block (“adipose tissue is exquisitely sensitive to the inhibitory effect of insulin on free fatty acid release.”*) the fat man on a high carbohydrate diet is nearly starving in the midst of plenty. Most of the carbohydrate he absorbs is turned into fat and accumulates in his fat stores and he cannot easily get it out again. The rest of the tissues of his body suffer a relative deprivation of nutriment and naturally he feels hungry and eats more. Habit, reinforced by the cheapness and ready availability of starchy and sugary foods, ensures that he attempts to satisfy his hunger with yet more carbohydrate which in turn forms more fat and still leaves him hungry. This vicious cycle goes on and he gets fatter.
(Mackarness 1958, added emphasis)22 *(Bonadonna 1990)23
Does muscle tone really matter for resting metabolic rates & health?
There’s a lot to explore here. If insulin resistance means that muscles can’t use available glucose, where does that excess energy go? What’s the effect of poor muscle tone on T2D? Or perhaps the obverse, how does sarcopenia (decline in muscle mass and functionality) impact T2D? We know what all the guidelines say about T2D: lose weight and exercise. There’s truth there, which this graph drives home.
How do we disassociate the effects of sarcopenia from those of T2D? Is there a feedback mechanism involved? And, is eating less and moving more the answer? Are there many approaches, all including exercise, to the eating portion of the equation to attain metabolic health?
Thinness or thickness?
If we think about it a bit, obesity in and of itself is not necessarily the worst portion of poor metabolic health (Lavie 2018).24 We know of normal-weight, metabolically-obese (NWMO) individuals, the so called thin-outside, fat-inside (TOFI) bodies. The problem here is fatty build-up in the liver, hepatic tissues, and their degradation. You might have heard one of the two types referred to, Non-Alcoholic Fatty Liver Disease (NAFLD) and Non-Alcoholic SteatoHepatitis (NASH), a destructive liver inflammation. You can be thin and metabolically challenged.
Is it metabolic syndrome or corpulence?
Metabolic syndrome (metS) uses waist circumference as one of its five risk measures. And body mass index (BMI) is strongly correlated to cardiovascular risk. (Hagg 2015)25 Additionally, obesity is an inflammatory condition.
Whoa, adipose tissue is like a hormonal gland?
Adipose (fat) tissue is an endocrine organ that influences metabolic processes and influences metabolic health. It does this when adipocytes secrete adipocytokines as an inflammatory response. (Barchetta 2019)26
What matters, losing weight or getting healthy?
Which leads us to question studies that focus on weight-loss without focusing on underlying metabolic health. (Hall 2020)27 How could epidemiological studies lead to useful information by incorporating metabolic markers? What can we take away from studies with obese subjects? What’s lipotoxicity? More importantly, what’s metabolic health? (Stroeve 2015)28
Frequent thirst (polydipsia) & urination (polyuria)?
These twin effects, symptoms that reveal themselves years before a medical diagnosis of diabetes is given, are synonyms for T2D. They are also intimately associated with kidney disease. Kidney disease is related to hypertension. The kidneys receive their signals indirectly from one of the body’s central controllers, the hypothalamus. This small region of the brain also controls hunger. Could it be one of the keys to regulating metabolic health?
But if snacking is the assumed modus vivendi, then thirst signals are being overwhelmed and even confused by feeding signals. Also, if excessive liquids, especially sweetened ones, are being consumed, then blood glucose and insulin will be abnormal. Not only that, but electrolytes are being affected as well.
Are subjects in studies participating with improper electrolyte balances? Aren’t those essential minerals important for metabolic health? Is diabetic bladder reversible?
Parting thoughts on part 1
I think there’s two takeaways from this section:
- DeFronzo’s graph showing the difference between metabolically healthy and inflexible muscle tissue glucose metabolic rates. For me this was an ‘aha moment’ for understanding T2D.
- Mackarness’s idea that corpulence is “starvation in the midst of plenty.” I think this insight will become an important metaphor for our Diabetes Dirge journey seeking metabolic health.
Nevertheless, you might feel a bit frustrated that I’ve left you with more questions about metabolic health than answers. Perhaps you already know the underlying issues and have answers. Hey, I don’t have most of the answers. But I promise to continue exploring this topic.
Let’s continue exploring together
Please post suggestions and comments to promote a productive discussion that furthers our thinking and learning together about metabolic health by answering these questions such as
- Was this discussion too technical?
- What was your key take away after reading this post?
If you enjoyed reading this you might try my other posts:
- Coronavirus quarantine – how a lifetime in submarines eases my use of isolation for self-improvement
- Pain started my ketogenic journey
Other resource guides & toolkits you might value
Curious about improving metabolic health with lifestyle?
- Lifestyle Medicine, the key to metabolic healing
- What is metabolic health? A layperson’s definition and a biochemist’s perspective
Where do I start improving my metabolic health?
- Your patient toolkit for prediabetes & type 2 diabetes
- What to eat? Get clever! Clinicians’ flexible approach to tailoring carb reduction to you.
- Want more detail on carbohydrate reduction? A round-up of quality, what-to-eat guides from around the web
- Best resources for an overview of keto – Metabolic Multiplier’s round up of the best resources we’ve found by evidence-based organizations & clinicians. For patients, families & caregivers.
- Keto doctors near me – over 20 directories of low-carb professionals
For clinicians using therapeutic carbohydrate reduction (TCR), ketogenic diet therapies (KDT)
- Best Keto resources for clinicians & other practitioners
- How to build my ketogenic therapy treatment team – Support for the more complex cases.
- Why write medical case reports about unique cases? – Our round up can save you time.
For colleagues interested in amplifying metabolic health
- Overview schematics help us think about metabolic health – Understand our Organizing Research team‘s thinking behind these 3 metabolic health research portals
- Communication guide to unite advocacy for metabolic health – Suggested language metabolic health advocacy. Principles. Language to use or avoid. Food & lifestyle first.
- Style Guide to unite advocacy for metabolic health – Welcome new team members! Many of you encourage using one voice for metabolic health. Below are suggestions from your fellow clinicians, scientists and professionals. See our Communication Guide as well. We’d love to hear…
- What Foundations support Metabolic Health? Charities, advocacy & grassroots groups using metabolic interventions & health to treat metabolic conditions.

This work is licensed under a Creative Commons Attribution 4.0 International License.
- Mechanick, J. I., Garber, A. J., Grunberger, G., Handelsman, Y., & Garvey, W. T. (2018). Dysglycemia-based chronic disease: an American Association of Clinical Endocrinologists position statement. Endocr Pract, 24(11), 995-1011. http://doi.org/ggtphz
- Kostoff, R. N. (2019). Prevention and reversal of chronic disease: lessons learned. http://hdl.handle.net/1853/62019
- Johnson, J. D., & Kushner, J. A. (2018). Endogenous insulin: its role in the initiation, progression and management of diabetes. The Endocrinologist, Autumn 2018(129). https://metmult.news/27d99
- van Ommen, B., et al. (2018). From diabetes care to diabetes cure-the integration of systems biology, ehealth, and behavioral change. Frontiers in Endocrinology, 8, 381. https://doi.org/gcx26s
- Bonadonna, R. C., Groop, L. C., Zych, K., Shank, M., & DeFronzo, R. A. (1990). Dose-Dependent Effect of Insulin on Plasma Free Fatty Acid Turnover and Oxidation in Humans. American Journal of Physiology-Endocrinology and Metabolism, 259(5), E736-E750. http://doi.org/dsk2
- Bysted, A., Hølmer, G., Lund, P., Sandström, B., & Tholstrup, T. (2005). Effect of dietary fatty acids on the postprandial fatty acid composition of triacylglycerol-rich lipoproteins in healthy male subjects. Eur J Clin Nutr, 59(1), 24-34. http://doi.org/bmjprw
- Lanese, N. (2019 July 15). What is homeostasis? Retrieved 2020 May 8 from https://www.livescience.com/65938-homeostasis.html
- Unwin, D., Haslam, D., & Livesey, G. (2016). It is the glycaemic response to, not the carbohydrate content of food that matters in diabetes and obesity: The glycaemic index revisited. Journal of Insulin Resistance, 1(1). http://doi.org/dt5s
- Glycated Insulin. (n.d.). R&D Systems. Retrieved 2020 May 6 from https://www.rndsystems.com/resources/articles/glycated-insulin
- DiNicolantonio, J. J., Mehta, V., Onkaramurthy, N., & O’Keefe, J. H. (2018). Fructose-induced inflammation and increased cortisol: A new mechanism for how sugar induces visceral adiposity. Prog Cardiovasc Dis, 61(1), 3-9. http://doi.org/gd49z2
- List of well over 100 different names for sugar. (n.d.) fabtrackr. Retrieved 2020 May 9 from https://fabtrackr.com/list-of-names-for-sugar/
- Substance Details, CAS Registry Number: 9050-36-6, CA Index Name: Maltodextrin. (n.d.). Common Chemistry. Retrieved 2020 May 9 from https://www.commonchemistry.org/ChemicalDetail.aspx?ref=9050-36-6
- Meugnier, E., Rome, S., & Vidal, H. (2007). Regulation of gene expression by glucose. Curr Opin Clin Nutr Metab Care, 10(4), 518-522. http://doi.org/dr3xh3
- Nilsson, P. M., Tuomilehto, J., & Rydén, L. (2019). The metabolic syndrome – what is it and how should it be managed? European Journal of Preventive Cardiology, 26(2_suppl), 33-46. http://doi.org/dsqf
- Feinman, R. D. (2012 February 2). Introduction to metabolism. The Black Box of life. Retrieved 2020 May 8 from https://feinmantheother.com/2012/02/02/648/
- Hue, L., & Taegtmeyer, H. (2009). The Randle cycle revisited: a new head for an old hat. American journal of physiology. Endocrinology and metabolism, 297(3), E578-E591. http://doi.org/ctpxx7
- Kelly, S. D., & Neary, S. L. (2020). Ominous Octet and Other Scary Diabetes Stories: The Overview of Pathophysiology of Type 2 Diabetes Mellitus. Physician Assistant Clinics, 5(2), 121-133. http://doi.org/dsqh
- Huber, M., et al. (2016). Towards a ‘patient-centred’ operationalisation of the new dynamic concept of health: a mixed methods study. BMJ Open, 6(1), e010091. http://doi.org/f3ndr9
- Wendimagegn, N. F., & Bezuidenhout, M. (2019). The integrated health service model: The approach to restrain the vicious cycle to chronic diseases. BMC health services research, 19(1), 347. http://doi.org/dsk7
- DeFronzo, R. A. (1988). Lilly lecture 1987. The triumvirate: β-Cell, muscle, liver: A collusion responsible for NIDDM. Diabetes, 37(6), 667-87.http://doi.org/dsk4[/efn_note] summarized his understanding of insulin on metabolism in this brilliant graph. Normal subjects and T2D sufferers received constant levels of insulin. What would you expect glucose usage levels to be for each group?

Metabolically healthy versus inflexible muscle glucose consumption with constant insulin. The graph is a summary of how many milligrams (mg) of glucose were consumed per each kilogram of body weight each minute with a constant insulin dose. The averages were 7 and 4 mg/kg-min for normal (metabolically healthy) and T2D (metabolically inflexible).
For 80 kg subjects (about 175 pounds) this results in 0.56 and 0.32 grams/min or 806 and 461 grams/day. In other words, T2D’s were only metabolizing 57% of the glucose that normal individuals were. Converting to calories/day using 4 calories/gram of carbohydrates the results are 3,224 calories/day for individuals without muscular insulin resistance and 1,644 calories/day for persons with metabolic illness.
Which one is not playing – the brain, gut, liver or muscle?
If the brain, gut and liver (splanchnic), fat (adipose) tissues are consuming the same amount of glucose from the blood, then the deficient glucose use is probably due to poor utilization by the muscles!
Starvation in the midst of plenty
Can you imagine if the individuals in this study had been snacking and feeding how much excess glucose the T2D individuals would have in their blood? Just think a bit about what adding food to a body that can’t use it means? T2D reveals its insidious nature: the diabetic is starving in the midst of plenty. (Salway 2017, original emphasis)20Salway, J. G. (2017). Metabolism at a glance (4th ed.). Wiley & Sons Ltd., 118
- Mackarness, R. (1958). Eat Fat and Grow Slim. The Harvill Press. 68
- Bonadonna, R. C., Groop, L. C., Zych, K., Shank, M., & DeFronzo, R. A. (1990). Dose-Dependent Effect of Insulin on Plasma Free Fatty Acid Turnover and Oxidation in Humans. American Journal of Physiology-Endocrinology and Metabolism, 259(5), E736-E750. http://doi.org/dsk2
- Lavie, C. J., Laddu, D., Arena, R., Ortega, F. B., Alpert, M. A., & Kushner, R. F. (2018). Healthy Weight and Obesity Prevention: JACC Health Promotion Series. Journal of the American College of Cardiology, 72(13), 1506-1531. http://doi.org/gfbdxm
- Hagg, S., et al. (2015). Adiposity as a cause of cardiovascular disease: a Mendelian randomization study. Int J Epidemiol, 44(2), 578-586. http://doi.org/f3n6kg
- Barchetta, I., Cimini, F. A., Ciccarelli, G., Baroni, M. G., & Cavallo, M. G. (2019). Sick fat: the good and the bad of old and new circulating markers of adipose tissue inflammation. Journal of Endocrinological Investigation. http://doi.org/gf9sxz
- Hall, K. D., et al. (2020). A plant-based, low-fat diet decreases ad libitum energy intake compared to an animal-based, ketogenic diet: An inpatient randomized controlled trial. Nutrixiv Preprints. http://doi.org/dt6k This is a case of confirmation bias: (1) the assumption that the patients were not diabetic was falsified by the OGTT (2) the OGTT high insulin levels after the ABLC subjects had been in ketosis shows they were metabolically inflexible (3) When in homeostasis the ABLC diet hsCRP, lactate, average and postprandial values were much better than the PBLC! ABLC = animal-based ketogenic low-carb diet, PBLF = plant-based low-fat diet, OGTT = oral glucose tolerance test
- Stroeve, J. H. M., et al. (2015). Phenotypic flexibility as a measure of health: the optimal nutritional stress response test. Genes & nutrition, 10(3), 13-13. http://doi.org/dt6h








Thank you for great article. Wish to add that during T2D an excess of insulin released also promotes release of the vasoconstrictor endothelin while Tumor Necrosis Factor alpha cytokine creating acute inflammation, decreases eNOS expression and stimulates von Willebrand Factor release. Looks like “perfect trio” for a CVA or PE…
Great insight. The choice is clear: activate inflammatory cascades or favorable metabolic signals. This recent article highlights the points you stressed: Balta, S. (2020). Endothelial dysfunction and inflammatory markers of vascular disease. Curr Vasc Pharmacol. https://doi.org/10.2174/1570161118666200421142542